الفرق بين المراجعتين لصفحة: «كودئين»
كنان الطرح (نقاش | مساهمات) (←مصادر) |
(قالب دواء، قالب أدوية سعال قالب أدوية إسهال، <!-- تضمين نص إنكليزي -->) |
||
| سطر 1: | سطر 1: | ||
{{Drugbox | |||
| English = Codeine | |||
| verifiedrevid = 456481929 | |||
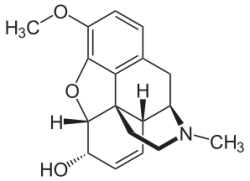
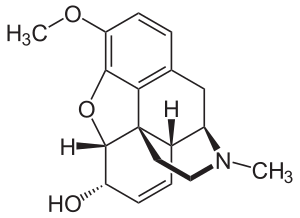
| IUPAC_name = (5α,6α)-7,8-didehydro-4,5-epoxy-3-methoxy-17-methylmorphinan-6-ol | |||
| image = Codein - Codeine.svg | |||
<!--Clinical data--> | |||
| tradename = | |||
| Drugs.com = {{drugs.com|monograph|codeine}} | |||
| MedlinePlus = a682065 | |||
| legal_AU = S8 | |||
| legal_CA = Schedule I | |||
| legal_UK = POM | |||
| legal_US = Schedule II | |||
| pregnancy_US = C | |||
| dependency_liability = High | |||
| routes_of_administration = Oral, intra-rectally, [[subcutaneous|SC]], [[intramuscular|IM]] | |||
<!--Pharmacokinetic data--> | |||
| bioavailability = ~90% Oral | |||
| metabolism = [[Liver|Hepatic]], via [[CYP2D6]] (cytochrome P450 2D6)<ref>{{Cite journal | author = Shen H, He MM, Liu H, ''et al'' | title = Comparative metabolic capabilities and inhibitory profiles of CYP2D6.1, CYP2D6.10, and CYP2D6.17 | journal = Drug Metab. Dispos. | volume = 35 | issue = 8 | pages = 1292–300 | year = 2007 | month = August | pmid = 17470523 | doi = 10.1124/dmd.107.015354 | url = }}</ref> | |||
| elimination_half-life = 2.5–3 h | |||
<!--Identifiers--> | |||
| CASNo_Ref = {{cascite|correct|CAS}} | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 76-57-3 | |||
| ATC_prefix = R05 | |||
| ATC_suffix = DA04 | |||
| ATC_supplemental = <br />combinations: {{ATC|N02|AA59}}, {{ATC|N02|AA79}} | |||
| PubChem = 5284371 | |||
| IUPHAR_ligand = 1673 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00318 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 4447447 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = Q830PW7520 | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = C06174 | |||
| ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| ChEBI = 16714 | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 485 | |||
<!--Chemical data--> | |||
| C=18 | H=21 | N=1 | O=3 | |||
| molecular_weight = 299.364 g/mol | |||
| smiles = CN1CC[C@]23c4c5ccc(c4O[C@H]2[C@H](C=C[C@H]3[C@H]1C5)O)OC | |||
| InChI = 1/C18H21NO3/c1-19-8-7-18-11-4-5-13(20)17(18)22-16-14(21-2)6-3-10(15(16)18)9-12(11)19/h3-6,11-13,17,20H,7-9H2,1-2H3/t11-,12+,13-,17-,18-/m0/s1 | |||
| InChIKey = OROGSEYTTFOCAN-DNJOTXNNBG | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C18H21NO3/c1-19-8-7-18-11-4-5-13(20)17(18)22-16-14(21-2)6-3-10(15(16)18)9-12(11)19/h3-6,11-13,17,20H,7-9H2,1-2H3/t11-,12+,13-,17-,18-/m0/s1 | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = OROGSEYTTFOCAN-DNJOTXNNSA-N | |||
}} | |||
<!-- | |||
'''Codeine''' or '''3-methylmorphine''' (a natural isomer of methylated [[morphine]]) is an [[opiate]] used for its [[analgesic]], [[Cough medicine|antitussive]], [[Antidiarrhoeal|antidiarrheal]], [[antihypertensive]], [[antianxiety]], [[sedative]] and [[hypnotic]] properties, to suppress premature [[Childbirth|labor]] contractions, [[myocardial infarction]], suppress coughing, as well as many other uses. Codeine is the second-most predominant [[alkaloid]] in [[opium]], at up to three percent. Although codeine can be extracted from natural sources, a [[semisynthesis|semi-synthetic]] process is the primary source of codeine for pharmaceutical use. It is considered the prototype of the weak to midrange [[opioids]] ([[tramadol]], [[dextropropoxyphene]], [[dihydrocodeine]], [[hydrocodone]], [[oxycodone]]). | |||
{{TOC limit|3}} | |||
==Medical uses== | |||
Codeine is used to treat mild to moderate [[pain]] and to relieve [[cough]].<ref name=AHFS>{{cite web|title=Codeine|url=http://www.drugs.com/monograph/codeine.html|work=The American Society of Health-System Pharmacists|accessdate=3 April 2011}}</ref> Codeine is also used to treat [[diarrhea]] and diarrhea predominant [[irritable bowel syndrome]], although [[loperamide]] (which is available [[Over-the-counter drug|OTC]] for milder diarrhea), [[diphenoxylate]], [[paregoric]] or even [[laudanum]] (also known as ''Tincture of Opium'') are more frequently used to treat severe diarrhea.<ref>{{cite book |title=Diarrhea: Diagnostic and Therapeutic Advances|publisher=Humana Press |date= November 8, 2010 | location = New York, USA|isbn=1-60761-182-1|page=452 |url=http://books.google.com/?id=BstHGdtpb9AC&printsec=frontcover&dq=Diarrhea:+Diagnostic+and+Therapeutic+Advances#v=onepage&q&f=false|author=Stefano Guandalini; Haleh Vaziri}}</ref> | |||
===Formulations=== | |||
Codeine is marketed as both a single-ingredient drug and in combination preparations with [[paracetamol]] (as [[co-codamol]]: ''e.g.,'' brands Paracod, Panadeine. Paramol, and the Tylenol-with-codeine series, including [[Tylenol 3]] and 1,2,4); with [[aspirin]]; (as [[co-codaprin]]); or with [[ibuprofen]] (as [[Nurofen Plus]]). These combinations provide greater pain relief than either agent alone (drug [[synergy]]). Codeine is also commonly marketed in products containing codeine with other pain killers or muscle relaxers, as well as codeine mixed with [[phenacetin]] (Emprazil With Codeine No. 1, 2, 3, and 4), [[naproxen]], [[indomethacin]], [[diclofenac]], and others, as well as more complex mixtures, including such mixtures as aspirin + paracetamol + codeine ± caffeine ± antihistamines and other agents, such as those mentioned above. | |||
Codeine-only products can be obtained with a prescription as a time release tablet (''e.g.,'' Codeine Contin 100 mg and Perduretas 50 mg). Codeine is also marketed in cough syrups with zero to a half-dozen other active ingredients, and a [[linctus]] (''e.g.,'' Paveral) for all of the uses for which codeine is indicated. | |||
Injectable codeine is available for subcutaneous or intramuscular injection; intravenous injection can cause a serious reaction that can progress to [[anaphylaxis]]. Codeine suppositories are also marketed in some countries. | |||
==Adverse effects== | |||
Common adverse effects associated with the use of codeine include [[drowsiness]] and [[constipation]]. Less common are [[Euphoria (emotion)|euphoria]], [[itching]], [[nausea]], [[vomiting]], [[dry mouth]], [[miosis]], [[orthostatic hypotension]], [[urinary retention]], [[Depression (mood)|depression]], and, paradoxically, [[coughing]]. Rare adverse effects include [[anaphylaxis]], [[Epileptic seizure|seizure]], and [[Hypoventilation|respiratory depression]].<ref>{{Cite web|publisher=WebMD LLC.|title=Codeine - adverse effects|url=http://reference.medscape.com/drug/codeine-343310#4|work=Medscape reference - Drugs, Diseases & Procedures|accessdate=27 Sep 2012}}</ref> As with all opiates, longer-term effects can vary but can include diminished libido, apathy and memory loss. Some people may also have an allergic reaction to codeine, such as the swelling of skin and rashes.<ref name=Drugs.com>[http://www.drugs.com/codeine.html Codeine Information from Drugs.com]</ref> | |||
Codeine and morphine as well as opium were used for control of diabetes until relatively recently, and still are in rare cases in some countries, and the hypoglycemic effect of codeine, although usually weaker than that of morphine, diamorphine, or hydromorphone, can lead to cravings for sugar. | |||
Tolerance to many of the effects of codeine develops with prolonged use, including therapeutic effects. The rate at which this occurs develops at different rates for different effects, with tolerance to the constipation-inducing effects developing particularly slowly for instance. | |||
A potentially serious adverse drug reaction, as with other opioids, is [[respiratory depression]]. This depression is dose-related and is the mechanism for the potentially fatal consequences of overdose. As codeine is metabolized to morphine, morphine can be passed through breast milk in potentially lethal amounts, fatally depressing the respiration of a breastfed baby.<ref>CTV News, [http://www.ctv.ca/servlet/ArticleNews/story/CTVNews/20080820/tylenol_3_breastfeeding_080820/20080820?hub=Canada Codeine use while breastfeeding may be dangerous], Wed. Aug. 20 2008 9:42 PM ET.</ref><ref>{{Cite journal|author=Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ |title=Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother |journal=Lancet |volume=368 |issue=9536 |page=704 |year=2006 |month=August |pmid=16920476 |doi=10.1016/S0140-6736(06)69255-6}}</ref> | |||
In August 2012, the Federal Drug Administration issued a warning about deaths in pediatric patients < 6 years old after ingesting "normal" doses of acetaminophen with codeine after tonsillectomy.<ref>{{cite web | url = http://www.fda.gov/Drugs/DrugSafety/ucm313631.htm#professionals | title = FDA Drug Safety Communication: Codeine use in certain children after tonsillectomy and/or adenoidectomy may lead to rare, but life-threatening adverse events or death | publisher = [[Food and Drug Administration]]}}</ref> Some patients are very effective converters of codeine to its active form, hydromorphone, resulting in lethal blood levels. The FDA presently is recommending very cautious use of Codeine in young tonsillectomy patients: use the drug in the lowest amount that can control the pain, use "as needed" and not "around the clock", and seek immediate medical attention if a child on codeine exhibits excessive sedation or abnormally noisy breathing. | |||
===Withdrawal and dependence=== | |||
As with other opiate-based pain killers, chronic use of codeine can cause [[physical dependence]]. When physical dependence has developed, withdrawal symptoms may occur if a person suddenly stops the medication. Withdrawal symptoms include: drug craving, runny nose, yawning, sweating, insomnia, weakness, stomach cramps, nausea, vomiting, diarrhea, muscle spasms, chills, irritability, and pain. To minimize withdrawal symptoms, long-term users should gradually reduce their codeine medication under the supervision of a healthcare professional.<ref>{{cite web| url = http://www.aadac.com/87_436.asp | title = The ABCs - Codeine and Other Opioid Painkillers | accessdate = Sep 12 2008 | author = Alberta Health Services | authorlink = Alberta Health Services | coauthors = AADAC | date = April 16, 2007 | publisher = Alberta Alcohol and Drug Abuse Commission }}</ref> | |||
Codeine is metabolized to [[codeine-6-glucuronide]] (C6G) by uridine diphosphate glucuronosyl transferase [[UGT2B7]], and, since only about 5% of codeine is metabolized by cytochrome P450 [[CYP2D6]], the current evidence is that C6G is the primary active compound.<ref>{{Cite journal|author=Armstrong SC, Cozza KL |title=Pharmacokinetic drug interactions of morphine, codeine, and their derivatives: theory and clinical reality, Part II |journal=Psychosomatics |volume=44 |issue=6 |pages=515–20 |year=2003 |pmid=14597688 |doi=10.1176/appi.psy.44.6.515}}</ref> Claims about the supposed "ceiling effect" of codeine doses are based on the assumption that high doses of codeine saturate CYP2D6, preventing further conversion of codeine to morphine, however it is now known that C6G is the main metabolite responsible for codeine's analgesia.<ref name="Vree2000">{{Cite journal|author=Vree TB, van Dongen RT, Koopman-Kimenai PM |title=Codeine analgesia is due to codeine-6-glucuronide, not morphine |journal=Int. J. Clin. Practa. |volume=54 |issue=6 |pages=395–8 |year=2000 |pmid=11092114 |doi=}}</ref> There is also no evidence that CYP2D6 inhibition is useful in treating codeine dependence,<ref>{{Cite journal|author=Fernandes LC, Kilicarslan T, Kaplan HL, Tyndale RF, Sellers EM, Romach MK |title=Treatment of codeine dependence with inhibitors of cytochrome P450 2D6 |journal=J Clin Psychopharmacol |volume=22 |issue=3 |pages=326–9 |year=2002 |month=June |pmid=12006904 |doi=10.1097/00004714-200206000-00014}}</ref> though the metabolism of codeine to morphine (and hence further metabolism to glucuronide morphine conjugates) does have an effect on the abuse potential of codeine.<ref>{{Cite journal|doi=10.1097/00004714-200008000-00008 |author=Kathiramalainathan K, Kaplan HL, Romach MK, ''et al.'' |title=Inhibition of cytochrome P450 2D6 modifies codeine abuse liability |journal=J Clin Psychopharmacol |volume=20 |issue=4 |pages=435–44 |year=2000 |pmid=10917405}}</ref> However, CYP2D6 has been implicated in the toxicity and death of neonates when codeine is administered to lactating mothers, particularly those with increased 2D6 activity ("ultra-rapid" metabolizers).<ref>{{Cite journal|pmid=16920476|author=Koren G, Cairns J, Chitayat D, Gaedigk A, Leeder SJ |title=Pharmacogenetics of morphine poisoning in a breastfed neonate of a codeine-prescribed mother|journal=Lancet |volume=368 |issue=9536 |page=704 |year=2006 |doi=10.1016/S0140-6736(06)69255-6}}</ref><ref>{{Cite journal|doi=10.1038/clpt.2009.151 |author=Willmann S, Edginton AN, Coboeken K, Ahr G, Lippert J |title=Risk to the Breast-Fed Neonate From Codeine Treatment to the Mother: A Quantitative Mechanistic Modeling Study|journal=Clinical Pharmacology & Therapeutics |volume=86 |issue=6 |pages=634–43 |year=2009}}</ref> | |||
==Pharmacokinetics== | |||
The conversion of codeine to morphine occurs in the liver and is catalysed by the [[cytochrome P450]] enzyme [[CYP2D6]]. [[CYP3A4]] produces norcodeine and [[UGT2B7]] conjugates codeine, norcodeine, and morphine to the corresponding 3- and 6- glucuronides. Approximately 6–10% of the Caucasians, 2% of Asians, and 1% of Arabs<ref>{{cite web|url=http://codeine.50g.com/info/codeine.html |title=Codeine Information - Facts - Codeine |accessdate=2007-07-16 |work=}}</ref> are "poor metabolizers"; they have little CYP2D6, and codeine is less effective for analgesia in these patients (Rossi, 2004). Srinivasan, Wielbo and Tebbett speculate that codeine-6-glucuronide is responsible for a large percentage of the analgesia of codeine, and, thus, these patients should experience some analgesia.<ref name="Srinivasan V, Wielbo D, Tebbett IR 1997 185–90">{{Cite journal|author=Srinivasan V, Wielbo D, Tebbett IR |title=Analgesic effects of codeine-6-glucuronide after intravenous administration |journal=European Journal of Pain |volume=1 |issue=3 |pages=185–90 |year=1997 |pmid=15102399 |doi=10.1016/S1090-3801(97)90103-8}}</ref> Many of the adverse effects will still be experienced in poor metabolizers. Conversely, 0.5-2% of the population are "extensive metabolizers"; multiple copies of the gene for 2D6 produce high levels of CYP2D6 and will metabolize drugs through that pathway more quickly than others. | |||
Some medications are CYP2D6 inhibitors and reduce or even completely block the conversion of codeine to morphine. The most well-known of these are two of the [[selective serotonin reuptake inhibitor]]s, [[paroxetine]] (Paxil) and [[fluoxetine]] (Prozac) as well as the antihistamine [[diphenhydramine]] and the antidepressant, [[bupropion]] (Wellbutrin, also known as Zyban). Other drugs, such as [[rifampicin]] and [[dexamethasone]], induce CYP450 isozymes and thus increase the conversion rate. | |||
Since codeine is a [[prodrug]], metabolism differences have the opposite effect. Thus an extensive metabolizer may have adverse effects from a rapid buildup of codeine metabolites while a poor metabolizer may get little or no pain relief. CYP2D6 is dysfunctional in 7% of white and black Americans, resulting in reduced metabolism of codeine. Other individuals may have two or more copies of the CYP2D6 gene, resulting in rapid metabolism of the target drug. CYP2D6 metabolizes and activates codeine into morphine, which then undergoes glucuronidation. Life-threatening intoxication, including respiratory depression requiring intubation, can develop over a matter of days in patients who have multiple functional alleles of CYP2D6, resulting in ultra-rapid metabolism of opioids such as codeine into morphine.<ref>{{Cite journal|author=Lurcott G |title=The effects of the genetic absence and inhibition of CYP2D6 on the metabolism of codeine and its derivatives, hydrocodone and oxycodone |journal=Anesth Prog |volume=45 |issue=4 |pages=154–6 |year=1998 |pmid=10483388 |pmc=2148980}}</ref><ref>{{Cite journal|author=Gasche Y, Daali Y, Fathi M, ''et al.'' |title=Codeine intoxication associated with ultrarapid CYP2D6 metabolism |journal=N. Engl. J. Med. |volume=351 |issue=27 |pages=2827–31 |year=2004 |month=December |pmid=15625333 |doi=10.1056/NEJMoa041888}}</ref><ref>{{Cite journal|author=Caraco Y |title=Genes and the response to drugs |journal=N. Engl. J. Med. |volume=351 |issue=27 |pages=2867–9 |year=2004 |month=December |pmid=15625340 |doi=10.1056/NEJMe048278}}</ref> | |||
The active metabolites of codeine, notably morphine, exert their effects by binding to and activating the μ-[[opioid receptor]]. | |||
==Relation to other opiates== | |||
Codeine is the starting material and prototype of a large class of mainly mild to moderately strong opioids such as [[hydrocodone]] (1920 in Germany), [[oxycodone]] (1916 in Germany), [[dihydrocodeine]] (1908 in Germany), and its derivatives such as [[nicocodeine]] (1956 in Austria). Other series of codeine derivatives include isocodeine and its derivatives, which were developed in Germany starting around 1920. As an analgesic, codeine [[Opiate comparison|compares moderately to other opiates]]. Related to codeine in other ways are [[codoxime]], [[thebacon]], [[Codeine-N-oxide|codeine-''N''-oxide]] (genocodeine), related to the nitrogen morphine derivatives as is codeine methobromide, and [[heterocodeine]], which is a drug six times stronger than morphine and 72 times stronger than codeine due to a small re-arrangement of the molecule, viz. moving the methyl group from the 3 to the 6 position on the morphine carbon skeleton. Drugs bearing resemblance to codeine in effects due to close structural relationship are variations on the methyl groups at the 3 position including [[ethylmorphine]] a.k.a. codethyline (Dionine) and [[benzylmorphine]] (Peronine). While having no narcotic effects of its own, the important opioid precursor [[thebaine]] differs from codeine only slightly in structure. Pseudocodeine and some other similar alkaloids not currently used in medicine are found in trace amounts in opium as well. | |||
==History== | |||
Codeine, or 3-methylmorphine, is an [[alkaloid]] found in the [[opium poppy]], ''Papaver somniferum var. album'', a plant in the [[papaveraceae]] family. Opium poppy has been cultivated and utilized throughout human history for a variety of medicinal (analgesic, anti-tussive and anti-diarrheal) and hypnotic properties linked to the diversity of its active components, which include morphine, codeine and [[papaverine]]. | |||
Codeine is found in concentrations of 0.9 to 3.0 per cent in opium prepared by the latex method from unripe pods of ''Papaver somniferum''. The name codeine is derived from the Greek word ''kodeia'' (κώδεια) for "poppy head". The relative proportion of codeine to morphine, the most common opium alkaloid at 4 to 23 per cent, tends to be somewhat higher in the poppy straw method of preparing opium alkaloids. | |||
Until the beginning of the 19th century, raw opium was used in diverse preparations known as [[laudanum]] (see [[Thomas de Quincey]]'s "[[Confessions of an English Opium-Eater]]", 1821) and [[paregoric]] [[elixir]]s, a number of which were popular in England since the beginning of the 18th century; the original preparation seems to have been elaborated in [[Leiden]], the [[Netherlands]] around 1715 by a chemist named Lemort; in 1721 the London Pharmocopeia mentions an Elixir Asthmaticum, replaced by the term Elixir Paregoricum ("pain soother") in 1746. | |||
The progressive isolation of opium's several active components opened the path to improved selectivity and safety of the opiates-based pharmacopeia. | |||
[[Morphine]] had already been isolated in [[Germany]] by German pharmacist [[Friedrich Sertürner]] in 1804.<ref>{{cite book|url=http://books.google.com/?id=MtOiLVWBn8cC&pg=PA20|page=20|title=Molecular, clinical and environmental toxicology|author=Andreas Luch|publisher=Springer|year=2009|isbn=3-7643-8335-6}}</ref> Codeine was first isolated decades later in 1832 in [[France]] by [[Pierre Jean Robiquet|Pierre Robiquet]], a French chemist and pharmacist already famous for the discovery of [[alizarin]], the most widespread red dye, while working on refined morphine extraction processes. This paved the way for the elaboration of a new generation of safer, codeine-based specific antitussive and antidiarrheal formulations. | |||
Codeine is currently the most widely-used opiate in the world,<ref name="opiates">[http://www.opiates.com/codeine/ Opiates.com - Codeine]</ref><ref name="sciencedaily">[http://www.sciencedaily.com/releases/2010/03/100314150916.htm Science Daily (March 2010) - "Unlocking the Opium Poppy's Biggest Secret: Genes That Make Codeine, Morphine"]</ref> and is one of the most commonly used drugs overall according to numerous reports by organizations including the World Health Organization and its League of Nations predecessor agency. It is one of the most effective orally administered opioid analgesics and has a wide safety margin. Its strength ranges from 8 to 12 percent of morphine in most people; differences in metabolism can change this figure as can other medications, depending on its route of administration. | |||
While codeine can be directly extracted from opium, its original source, most codeine is synthesized from the much more abundant [[morphine]] through the process of O-[[methylation]].<ref name="sciencedaily" /><ref>[http://www.elmhurst.edu/~chm/vchembook/674narcotic.html Elmhurt College - Narcotic Analgesic Drugs]</ref> | |||
By 1972, the effects of the [[War On Drugs|Nixon War On Drugs]] had caused across-the-board shortages of illicit and licit opiates because of a scarcity of natural opium, poppy straw, and other sources of opium alkaloids, and the geopolitical situation was growing difficult for the United States. After a large percentage of the opium and morphine in the [[Defense National Stockpile Center|US National Stockpile of Strategic & Critical Materials]] was tapped in order to ease severe shortages of medicinal opiates — the codeine-based antitussives in particular — in late 1973, researchers were tasked with finding a way to synthesize codeine and its derivatives. They quickly succeeded using petroleum or coal tar and a process developed at the United States' National Institutes of Health. | |||
Numerous codeine salts have been prepared since the drug was discovered. The most commonly used are the hydrochloride (freebase conversion ratio 0.805), phosphate (0.736), sulphate (0.859), and citrate (0.842). Others include a [[salicylate]] [[NSAID]], codeine salicylate (0.686), and at least four codeine-based [[barbiturates]], the cyclohexenylethylbarbiturate (0.559), cyclopentenylallylbarbiturate (0.561), diallylbarbiturate (0.561), and diethylbarbiturate (0.619). | |||
==Recreational use== | |||
Codeine can be used as a [[recreational drug]]. | |||
In some countries, cough syrups and tablets containing codeine are available without prescription; some potential recreational users are reported to buy codeine from multiple pharmacies so as not to arouse suspicion. A heroin addict may use codeine to ward off the effects of a [[withdrawal]].<ref>{{Cite book| last = Boekhout van Solinge | first = Tim | title = L'héroïne, la cocaïne et le crack en France. Trafic, usage et politique | publisher = CEDRO Centrum voor Drugsonderzoek, Universiteit van Amsterdam | location = Amsterdam | language = French | pages = 247–262 | chapter = 7. La politique de soins des années quatre-vingt-dix | chapterurl = http://www.cedro-uva.org/lib/boekhout.heroine.fr.7.html | year = 1996}}</ref> | |||
Codeine is also available in conjunction with the anti-nausea medication [[promethazine]] in the form of a syrup. Brand named as Phenergan with Codeine or in generic form as promethazine with codeine. Called '[[Purple drank|syrup]]', this medication is quickly becoming one of the most commonly misused codeine preparations.<ref>{{Cite news|publisher = [[USA Today]] |first = Donna | last = Leinwand |title = DEA warns of soft drink-cough syrup mix | url = http://www.usatoday.com/news/nation/2006-10-18-lean_x.htm?csp=34 |date = 2006-10-18 |accessdate = 2006-10-23}}</ref> Rapper [[Pimp C]], from the group [[UGK]], died from an overdose of this combination.<ref>http://www.chron.com/entertainment/music/article/Pimp-C-s-death-caused-by-overdose-and-sleep-1629962.php</ref> | |||
Codeine is also demethylated by reaction with [[pyridine]] to illicitly synthesize morphine, which can then be acetylated to make heroin (diacetylmorphine). Pyridine is toxic and possibly [[carcinogenic]], so morphine illicitly produced in this manner (and potentially contaminated with pyridine) may be particularly harmful.<ref>{{Cite book| last = Hogshire | first = Jim | authorlink = Jim Hogshire | title = Pills-A-Go-Go: A Fiendish Investigation into Pill Marketing, Art, History & Consumption | publisher = Feral House | year = 1999 | month = June | location = Los Angeles | pages = 216–223 | isbn = 978-0-922915-53-8}}</ref> Codeine can also be turned into [[α-chlorocodide]], which is used in the clandestine synthesis of [[desomorphine]] (Permonid) (desomorphine attracted attention in 2010 in [[Russia]] due to an upsurge in clandestine production, presumably due to its relatively simple synthesis from codeine.{{Citation needed|date=November 2011}} The drug is easily made from codeine, [[iodine]] and [[red phosphorus]],<ref>{{cite journal |pages=361–70 |doi=10.1134/S1061934808040096 |title=Chromatographic study of expert and biological samples containing desomorphine |year=2011 |last1=Savchuk |first1=S. A. |last2=Barsegyan |first2=S. S. |last3=Barsegyan |first3=I. B. |last4=Kolesov |first4=G. M. |journal=Journal of Analytical Chemistry |volume=63 |issue=4}}</ref> in a similar process to the manufacture of [[methamphetamine]] from [[pseudoephedrine]], but desomorphine made this way is highly impure and contaminated with various toxic and corrosive byproducts.). | |||
===Detection=== | |||
Codeine and/or its major metabolites may be quantitated in blood, plasma or urine to monitor therapy, confirm a diagnosis of poisoning or assist in a medicolegal death investigation. Drug abuse screening programs generally test urine, hair, sweat or oral fluid. Many commercial opiate screening tests directed at morphine cross-react appreciably with codeine and its metabolites, but chromatographic techniques can easily distinguish codeine from other opiates and opioids. It is important to note that codeine usage results in significant amounts of morphine as an excretion product. Furthermore, heroin contains codeine (or acetylcodeine) as an impurity and its use will result in excretion of small amounts of codeine. Poppy seed foods represent yet another source of low levels of codeine in one's biofluids. Blood or plasma codeine concentrations are typically in the 50–300 µg/L range in persons taking the drug therapeutically, 700–7000 µg/L in chronic users and 1000–10,000 µg/L in cases of acute fatal overdosage.<ref>{{cite journal |author=Thevis M, Opfermann G, Schänzer W |title=Urinary concentrations of morphine and codeine after consumption of poppy seeds |journal=J. Anal. Toxicol. |volume=27 |pages=53–6 |year=2003 |pmid=12587685 |issue=1}}</ref><ref>{{cite journal |author=Cone EJ, Welch P, Paul BD, Mitchell JM |title=Forensic drug testing for opiates, III. Urinary excretion rates of morphine and codeine following codeine administration |journal=J. Anal. Toxicol. |volume=15 |pages=161–6 |year=1991 |pmid=1943064 |issue=4}}</ref><ref>{{cite book |author=Baselt, R. |title=Disposition of Toxic Drugs and Chemicals in Man |publisher=Biomedical Publications |location=Foster City CA |year=2008 |pages=355–360 |edition=8th }}</ref> | |||
==Legal status== | |||
In [[Australia]], [[Canada]], [[New Zealand]], [[Romania]], [[Russia]], [[Sweden]], the [[United Kingdom]], the [[United States]], and many other countries, codeine is regulated under various [[Drug prohibition law#List by jurisdiction of principal drug prohibition laws|narcotic control laws]]. In some countries it is available without prescription in combination preparations from licensed pharmacists in doses up to 15 mg/tablet in Australia, New Zealand, Poland, Romania (Codamin), and Costa Rica, 12.8 mg/tablet in the UK, 10 mg/tablet in Israel and 8 mg/tablet in Canada and Estonia.{{Citation needed|date=June 2007}}<!--I did find this unsupported reference "it is available without prescription in combination preparations from licensed pharmacists in doses up to 8 mg/tablet in Canada and Australia, 15 mg/tablet in New Zealand and 12.8mg/tablet in Ireland and the UK (with paracetamol or ibuprofen), 9.6 mg/tablet in Denmark (with acetylosalicic acid and magnesium hydroxide making it unfit for cold water extraction). For Ireland, the ceiling is 20 mg per doseage unit. "-->. | |||
<!-- | |||
===Australia=== | |||
In Australia, codeine preparations must be sold only at a pharmacy. Preparations will often be a combination of paracetamol (500 mg), ibuprofen (200 mg) and doxylamine succinate (5 mg), and the codeine content may range from 5 mg to 15 mg; preparations with in excess of 30 mg per tablet are S4 (schedule 4, or Prescription Only) medications. The item is given over the counter, no prescriptions, at the discretion of the Pharmacist. Most preparations are considered S3 (schedule 3, or Pharmacist Only) medications, meaning that they must be sold with the direct involvement of a pharmacist. It must be labelled and usage history monitored by the Pharmacist to help deter misuse and dependence. The exception to this rule is cold and flu preparations such as "Codral". These preparations contain phenylephrine (5 mg), paracetamol(500 mg) and codeine(9.5 mg).<ref>{{cite web| title = Codeine crackdown comes into effect | publisher = ABC.net.au | url = http://www.abc.net.au/news/stories/2010/05/01/2887640.htm | accessdate = 2010-11-22 }}</ref><br /> | |||
Preparations containing pure codeine (e.g., codeine phosphate tablets or codeine phosphate [[linctus]]) are available on prescription and are considered S8 (schedule 8, or Controlled Drug (Possession without authority illegal)). [[Standard for the Uniform Scheduling of Medicines and Poisons#Schedule 8 Controlled Drug (Possession without authority illegal)|Schedule 8]] preparations are subject to the strictest regulation of all medications available to consumers. | |||
===Denmark=== | |||
In Denmark codeine is sold over the counter with max 9.6 mg in mixture. The item is given over the counter, no prescriptions. The strongest available over the counter preparation containing codeine has 9.6 mg (with aspirin, brand name Kodimagnyl); anything stronger requires a prescription. | |||
===France=== | |||
In [[France]], most preparations containing codeine do not require a doctor's prescription. Example products containing codeine include Néocodion (cough pills, ad sirup), Codoliprane (codeine with paracetamol), Prontalgine and Migralgine (codeine, paracetamol and caffeine).<ref>{{cite web| title = vital list of codein | publisher = vidal.com | url = http://www.vidal.fr/Substance/codeine-1039.htm |accessdate = 2011-01-12 }}</ref> | |||
===Germany, Switzerland and Austria=== | |||
Codeine is listed under the ''[[Betäubungsmittelgesetz]]'' in [[Germany]] and the similarly named narcotics and controlled substances law in [[Switzerland]]. In [[Austria]], the drug is listed under the ''[[Suchtmittelgesetz]]'' in categories corresponding to their classification under the Single Convention on Narcotic Drugs. Dispensing of products containing codeine and similar drugs ([[dihydrocodeine]], nicocodeine, benzylmorphine, ethylmorphine etc.), in general, requires a prescription order from a doctor or the discretion of the pharmacist. Municipal and provincial regulations may impact availability, in particular in Austria and Switzerland, which allows cities and provinces to regulate the selling of the least-regulated schedule of the SMG/BtMG; and, of course, individual chemists' shops can opt out of providing them or imposing volume, frequency, or single-purchase limitations and other things of the same store. Plain codeine hydrochloride tablets (which in the USA would share CSA Schedule II with drugs like morphine, cocaine, hydromorphone, and bezitramide) as well as other non-injectable forms of codeine and its midrange derivatives can be dispensed in this way; the same goes for most chemical classes of benzodiazepines, the majority of non-barbiturate sedative/hypnotics, and at least a handful of barbiturates. | |||
Title 76 of the [[Schengen treaty]] has made it possible for countries within the signatory states to import and export drugs with various provisos, recording and ordering requirements, and various other rules. | |||
===Greece=== | |||
Codeine is classed as an illegal drug in Greece, and individuals possessing it could conceivably be arrested, even if they were legitimately prescribed it in another country. It is sold only with a doctor's prescription (Lonarid-N, Lonalgal).<ref>{{cite web| title = Pharmacies in Greece | publisher = About.com | url = http://gogreece.about.com/od/planagreattriptogreece/a/greecepharmacy_2.htm | accessdate = 2009-10-10 }}</ref> | |||
===Hong Kong=== | |||
In [[Hong Kong]], codeine is regulated under Schedule 1 of Hong Kong's Chapter 134 ''Dangerous Drugs Ordinance''. It can be used legally only by health professionals and for university research purposes. The substance can be given by pharmacists under a prescription. Anyone who supplies the substance without prescription can be fined $10,000 ([[Hong Kong dollar|HKD]]). The maximum penalty for trafficking or manufacturing the substance is a $5,000,000 (HKD) fine and life imprisonment. Possession of the substance for consumption without license from the Department of Health is illegal with a $1,000,000 (HKD) fine and/or 7 years of jail time. | |||
However, codeine is available without prescription from licensed pharmacists in doses up to 0.1% (5 mg/5ml) according to Hong Kong "Dangerous Drugs Ordinance". | |||
===Iceland=== | |||
Preparations of [[paracetamol]] and codeine require a prescription in Iceland. These tablets are known as ''Parkódín''. | |||
===India=== | |||
Codeine preparations require a prescription in India. A preparation of [[paracetamol]] and codeine is available in India. Codeine is also present in various cough syrups as Codeine Phosphate. | |||
===Ireland=== | |||
In the [[Republic of Ireland]], new regulations came into effect on August 1, 2010<ref>{{cite news | url = http://www.irishtimes.com/newspaper/health/2010/0824/1224277436013.html | publisher = The Irish Times | date = 08 Aug 2010 | title = Codeine regulations cause a few headaches}}</ref> concerning codeine, due to worries about the overuse of the drug. Codeine remains a semi non-prescriptive, over-the-counter drug up to a limit of 12.8 mg per pill, but codeine products must be out of the view of the public to facilitate the legislative requirement that these products “are not accessible to the public for self-selection”.<ref>[http://www.attorneygeneral.ie/esi/2008/B26511.pdf Office of The Attorney General, Regulation 5(1)(e) of the Regulation of Retail Pharmacy Businesses Regulations 2008 (S.I. 488 of 2008)]</ref> In practice, this means customers must ask pharmacists for the product containing codeine in name, and the pharmacist makes a judgement whether it is suitable for the patient to be using codeine, and that patients are fully advised of the correct use of these products. Products containing more than 12.8 mg codeine are available on prescription only.<ref>{{cite document | url = http://www.thepsi.ie/Libraries/Consultations/Draft_Codeine_Guidelines.sflb.ashx | title = Non-Prescription Medicinal Products Containing Codeine: Draft Guidance for Pharmacists | publisher = [[Pharmaceutical Society of Ireland]]}}</ref> | |||
===Italy=== | |||
Codeine tablets or preparations require a prescription in Italy. A preparation of [[paracetamol]] and codeine is available in Italy as ''CoEfferalgan''. | |||
===Japan=== | |||
Codeine and similar mid-level centrally acting agents in combination with non-opioid analgesics, antihistamines, vitamins, inert GI agents like kaolin & pectin, mild laxatives, antacids, and herbal preparations, can be purchased over the counter, with 10 mg being the ceiling for OTC dispensing. This is also true of ethylmorphine and dihydrocodeine, and also diphenoxylate, some weak relatives of the thiambutene opioid family. | |||
===Russia=== | |||
According to ITAR-Tass and Austria Presse-Agentur, OTC availability of codeine products was rescinded nationwide in 2012 because of the discovery of the Krokodil method of underground desomorphine synthesis. Opponents of the move point out that codeine has not been available OTC in 22 of Russia's oblasts for years and the demand will call forth its own supply, meaning that only legitimate end users are negatively impacted (activist quoted in Pravda story on issue) | |||
===Sri Lanka=== | |||
Codeine preparations are available as over the counter pharmacy medicines in Sri Lanka. The most common preparation is Panadeine, which contains 500 mg of Paracetamol and 8 mg of Codeine. | |||
===North America=== | |||
====Narcotic content numbers==== | |||
Narcotic content number in the US names of codeine tablets and combination products like Tylenol With Codeine No. 3, Emprin With Codeine No. 4, and pure codeine tablets are as follows: No. 1 - 7½ or 8 mg (1/8 grain), No. 2 - 15 or 16 mg (1/4 grain), No. 3 - 30 or 32 mg (1/2 grain), No. 4 - 60 or 64 mg (1 grain). The Canadian "Frosst 222"<ref>[http://www.lib.uwo.ca/programs/companyinformationcanada/Merck.html Business and History - Merck Frosst Canada Inc. | Western Libraries]</ref> series is identical to the above list: "222" contains 8 mg codeine, "282" 15 mg, "292" 30 mg, and "293" 60 mg. This system, which is also used at present in the trade names of some [[dihydrocodeine]] and [[ethylmorphine]] products both in and outside of North America, was inaugurated with the [[Pure Food and Drug Act]] of 1906 and related legislation and refined since. | |||
Equivalent scales for labeling stronger opioids such as [[diacetylmorphine]] (heroin), [[morphine]], opium salts mixtures, and others were in common use in the past, and on occasion one can find past references to brand names for [[hydrocodone]] (invented 1920, introduced in US 1943), [[hydromorphone]] (invented 1924), [[oxycodone]] (invented 1916), [[paregoric]] and similar drugs containing narcotic content numbers. For example. from circa 1900 to 1925, the most common cough medicine was [[terpin hydrate]] With Heroin Elixir No. 2. | |||
Contrary to the advertising matter of some pharmacies, 60 mg is No. 4, not No. 6, and tablets with 45 mg of codeine are not No. 4 and would in all likelihood be classified as No. 3½ under that system. Whether the scale goes to No. 5 and higher is moot at this point, as in the United States and Canada single-dose-unit concentrations of more than 64 mg are not manufactured. The United States [[Controlled Substances Act]] of 1970 does place dosage unit strengths of 90 mg of codeine and higher in Schedule II, even if mixed with another active ingredient. Oral tablets, hypodermic tablets, liquid forms, and capsules of less common doses are available in some cases the equivalent dihydrocodeine, [[dionine]], [[benzylmorphine]], and opium dosages were previously available in North America (and in most cases still are in other countries, particularly the 45 mg paracetamol/codeine and 50 and 100 mg single-ingredient codeine tablets). | |||
====United States==== | |||
In the [[United States]], codeine is regulated by the [[Controlled Substances Act]]. It is a Schedule II controlled substance for pain-relief products containing codeine alone or more than 90 mg per dosage unit. Tablets of codeine in combination with aspirin or acetaminophen ([[paracetamol]]/Tylenol) made for pain relief are listed as Schedule III; and cough syrups are Schedule III or V, depending on formula. The acetaminophen/codeine pain-relief elixir (trade name Tylenol Elixir with Codeine) is a Schedule IV controlled substance.<ref name="Valeant Pharmaceuticals Prescribing Information for Capital with Codeine Oral Suspension">{{cite web| author =Valeant Pharmaceuticals | authorlink =Valeant Pharma | url =http://www.valeant.com/fileRepository/products/PI/Capital_with_Codeine_Suspension_120mg_PI_Aug04.pdf| title =Prescribing Information for Capital with Codeine (acetaminophen with codeine) showing Schedule V designation | format =PDF | accessdate =2011-02-25}}</ref> | |||
Preparations for cough or diarrhea containing small amounts of codeine in combination with two or more other active ingredients are Schedule V in the US, and in some states may be dispensed in amounts up to 4 fl. oz. per 48 hours (one or two states set the limit at 4 fl. oz. per 72 hours) without a prescription. Schedule V specifically consigns the product to state and local regulation beyond certain required record-keeping requirements (a dispensary log must be maintained for two years in a ledger from which pages cannot easily be removed and/or are pre-numbered, and the pharmacist must ask for photo identification) and also maintain controlled substances in the closed system at the root of the régime intended by the Controlled Substances Act of 1970; the codeine in these products was a Schedule II substance when the company making the Schedule V product acquired it for mixing up the end-product. | |||
In locales where dilute codeine preparations are non-prescription, anywhere from very few to perhaps a moderate percentage of pharmacists will sell these preparations without a prescription. However, many states have their own laws that do require a prescription for Schedule V drugs. The December 2008 issue of ''The Bulletin of the National Codeine OTC Lobby'' (Vol. XVIII, No. 4) listed 12 states with some kind of OTC access to codeine, noting that small independent pharmacies are the most likely to have it. This situation is roughly equivalent to that in February 1991, when the aforementioned organisation undertook its first comprehensive study of Schedule V and overall codeine, dihydrocodeine, ethylmorphine, and hydrocodone availability. | |||
Other drugs that are present in Schedule V narcotic preparations like the codeine syrups are [[ethylmorphine]] and [[dihydrocodeine]]. [[Paregoric]] and hydrocodone were transferred to Schedule III from Schedule V even if the preparation contains two or more other active ingredients, and [[diphenoxylate]] is usually covered by state prescription laws even though this relative of [[pethidine]] is a Schedule V substance when adulterated with atropine to prevent abuse. | |||
Around the world, codeine is, contingent on its concentration, a Schedule II and III drug under the [[Single Convention on Narcotic Drugs]].<ref name="INCB-Yellow">{{cite web| author =International Narcotics Control Board | authorlink =International Narcotics Control Board | url =http://www.incb.org/pdf/e/list/46thedition.pdf | title =List of Narcotic Drugs under International Control | format =PDF | accessdate =2006-05-24}}</ref> | |||
===Spain=== | |||
Codeine tablets or preparations require a prescription in Spain, although this is often not enforced and many pharmacies will sell codeine products without the requirement of a prescription.{{Citation needed|date=March 2011}} | |||
===United Kingdom=== | |||
In the [[United Kingdom]], neat codeine and higher-strength codeine formulations - such as 30/500 co-codamol (where 30 mg of codeine phosphate is combined with 500 mg [[paracetamol]]) are prescription-only medicines (POM). Lower-strength combinations, such as 8/500 (various brands) or 12.8/500 (Panadol Ultra, Solpadeine MAX and others) are available as pharmacy medicines over the counter. Codeine is also available combined with [[Ibuprofen]]; a common formulation is 12.8 mg codeine alongside 200 mg Ibuprofen. It is also available 'behind the counter' with aspirin in doses of 8 mg codeine phosphate and 500 mg [[aspirin]] (Codis). Codeine Linctus of 15 mg per 5ml is also available behind the counter at some pharmacies, although a purchaser would have to request it specifically from the pharmacist. | |||
Under the Misues of Drugs Act 1971, possession of codeine is legal without a prescription in quantities of up to 12.5 mg when in tablet form. As with most opioids, possession of neat codeine without a prescripion is illegal in quantities over 12.5 mg and is currently a class B controlled drug. However, if it prepared for intra-muscular injection, it is then considered to be a class A controlled drug. Thus it is legal for a person to carry neat codeine in quantities over 12.5 mg assuming that they possess a valid prescription, subject to the quantities carried being for personal use only and with no indication that there is intent to supply.<ref>http://www.legislation.gov.uk/ukpga/1971/38/schedule/2</ref> | |||
==References== | |||
{{Reflist|2}} | |||
{{Opioids}} | |||
{{Analgesics}} | |||
{{Antidiarrheals, intestinal anti-inflammatory/anti-infective agents}} | |||
{{Cough and cold preparations}} | |||
[[Category:French inventions]] | |||
[[Category:Antitussives]] | |||
[[Category:Antidiarrhoeals]] | |||
[[Category:Natural opium alkaloids]] | |||
[[Category:World Health Organization essential medicines]] | |||
[[Category:Phenol ethers]] | |||
[[Category:Morphinans]] | |||
[[Category:Alkenes]] | |||
[[Category:Opiates]] | |||
[[Category:Prodrugs]] | |||
--> | |||
'''الكودئين Codeine''' هو ميتيل مورفين، كودئين فوسفات، كودئين سلفات. | '''الكودئين Codeine''' هو ميتيل مورفين، كودئين فوسفات، كودئين سلفات. | ||
[[ملف:Codein.png|thumb|250px]] | [[ملف:Codein.png|thumb|250px]] | ||
| سطر 82: | سطر 308: | ||
*أقراص ذوابة: 15ملغ، 30ملغ، 60ملغ | *أقراص ذوابة: 15ملغ، 30ملغ، 60ملغ | ||
==مصادر== | ==مصادر== | ||
{{ثبت المراجع}} | |||
كتاب الشامل في الأدوية السريرية، د.محمد عبد الرحمن العينية - د.محمود موسى طلوزي، منشورات دار القدس للعلوم | كتاب الشامل في الأدوية السريرية، د.محمد عبد الرحمن العينية - د.محمود موسى طلوزي، منشورات دار القدس للعلوم | ||
| سطر 87: | سطر 314: | ||
{{أفيونات}} | {{أفيونات}} | ||
{{مسكنات}} | {{مسكنات}} | ||
{{Antidiarrheals, intestinal anti-inflammatory/anti-infective agents}} | |||
{{Cough and cold preparations}} | |||
[[تصنيف:أدوية]] | [[تصنيف:أدوية]] | ||
[[تصنيف:موسوعة الأدوية]] | [[تصنيف:موسوعة الأدوية]] | ||
[[تصنيف:مسكنات]] | [[تصنيف:مسكنات]] | ||
[[تصنيف:أفيونات]] | [[تصنيف:أفيونات]] | ||
مراجعة 08:39، 26 أبريل 2013
| |
|---|---|
| Systematic (IUPAC) name | |
| (5α,6α)-7,8-didehydro-4,5-epoxy-3-methoxy-17-methylmorphinan-6-ol | |
| Clinical data | |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a682065 |
| Pregnancy cat. | C (US) |
| Legal status | Controlled (S8) (AU) Schedule I (CA) POM (UK) Schedule II (US) |
| Dependence liability | High |
| Routes | Oral, intra-rectally, SC, IM |
| Pharmacokinetic data | |
| Bioavailability | ~90% Oral |
| Metabolism | Hepatic, via CYP2D6 (cytochrome P450 2D6)[1] |
| Half-life | 2.5–3 h |
| Identifiers | |
| CAS number | 76-57-3 |
| ATC code | R05DA04 combinations: N02AA59, N02AA79 |
| PubChem | CID 5284371 |
| IUPHAR ligand | 1673 |
| DrugBank | DB00318 |
| ChemSpider | 4447447 |
| UNII | Q830PW7520 |
| KEGG | C06174 |
| ChEBI | CHEBI:16714 |
| ChEMBL | CHEMBL485 |
| Chemical data | |
| Formula | C18H21NO3 |
| Mol. mass | 299.364 g/mol |
| |
| |
| | |
.
الكودئين Codeine هو ميتيل مورفين، كودئين فوسفات، كودئين سلفات.
الزمرة الدوائية
مسكن أفيوني ومضاد سعال
الاستعمال
علاج الألم الخفيف إلى متوسط الشدة، وكمضاد سعال بجرعته المنخفضة.
الاستخدام خلال الحمل
ينتمي لأدوية المجموعة C، وينتمي بأدوية المجموعة D إذا استخدم لفترات طويلة أو بجرعات منخفضة.
مضادات الاستطباب
فرط الحساسية له أو لمكوناته.
تحذيرات
- استخدامه بحذر عند مرضى فرط الحساسية للشادات الأفيونية المشتقة من مجموعة فينانترين (مورفين هيدروكلوريد، هيدرومورفون، أوكسي كودون، أوكسي مورفون) أو المصابين بأحد الأمراض التنفسية كالربو أو النفاخ أو الداء الرئوي أو الساد المزمن أو المصابين بمرض شديد كبدي أو كلوي.
- قد تحوي بعض مستحضراته مادة السلفيت التي قد تسبب ارتكاست أرجية ملحوظة الشدة.
- لا ينصح باستخدامه لتثبيط السعال المنتج للقشع، ولا ينصح باستخدامه لتثبيط السعال عند الأطفال الذين تقل أعمارهم عن سنتين.
- قد يكون المريض المسن مؤهب بشكل كبير للإصابة بالتخليط والإمساك والتأثيرات المثبطة العصبية المركزية بقية التأثيرات الجانبية الناجمة عن الشادات الأفيونية.
الآثار الجانبية
- بنسبة تزيد عن 10%:
- قلبية وعائية: بطء/تسرع القلب، انخفاض التوتر الشرياني.
- عصبية مركزية: دوام، خفة الرأس، شعور كاذب بالتحسن، تعب، صداع، تململ تنبه عصبي مركزي تناقصي، تخليط.
- جلدية: شرى، طفح
- هضمية: جفاف الفم، قهم، غثيان، إقياء
- بولية تناسلية: نقص التبول، تشنج حالبي
- موضعية: حس حرق عند موضع الحقن
- عينية: تشوش الرؤية
- عصبية عضلية: ضعف عضلي
- تنفسية: زلة تنفسية
- متنوعة: تحرر الهيستامين
- بنسبة تقل عن 10%:
- عصبية مركزية: اختلاجات، إهلاس، اكتئاب، كوابيس، أرق
- هضمية: علوص شللي، تشنج صفراوي، معص معدي
فرط الجرعة/الانسمام
- تثبيط تنفسي وعصبي مركزي ومعص هضمي وإمساك.
- النالوكسون ترياق نوعي يستخدم للتدبير، يعطى حقناً وريدياً بجرعة 2ملغ (قد يستطب تكرارها عدة مرات) ، الجرعة القصوى 10ملغ.
التداخلات الدوائية
- تنخفض شدة التأثير عند المدخنين
- تزداد الفعالية والسمية عند إشراكه مع مثبطات الجملة العصبية والفينزتيازيدات أو TCAs أو أحد الشادات الأفيونية الأخرى أو غوانابنز أو مثبطات MAO أو المرخيات العضلية
الثبات
- يحفظ بدرجة 15-30م ولا يعرض للتجمد أو الضوء
- لا يستخدم محلوله المعد للحقن فيما و تغير لونه أو تحوصب
الآلية
-يرتبط مع المستقبلات الأفيونية في CNS مما يؤدي لحصار التوصيل عبر سبل الألم الصاعدة، كذلك فهو يؤثر على شدة الإحساس بالألم والارتكاس له. -يثبط السعال بالتأثير المباشر المركزي على البصلة السيسائية -ي4سبب تثبيط عصبي مركزي معمم.
الحرائك الدوائية
- بدء التأثير:
- فموي: 0.5-1 ساعة
- حقن عضلي: 10-30 دقيقة
- ذروة التأثير:
- فموي: 1-1.5 ساعة
- حقن عضلي: 0.5-1 ساعة
- مدة التأثير: 4-6 ساعات
- الامتصاص: كافي يلي تناوله عبر الفم
- التوزع: يعبر المشيمة، ويهر في حليب الأم
- الارتباط البروتيني: 7%
- الاستقلاب: يستقلب في الكبد متحولاً إلى مورفين
- العمر النصفي: 2.5-3.5 ساعة
- الإطراح: يطرح 3% إلى 16% مع البول على شكل دواء غير متبدل ونوركودئين ومورفين حر ومورفين مرتبط.
الجرعة
- يجب معايرة الجرعات حسب التأثير التسكيني المطلوب، إن نسبة فعالية الجرعة الفموية المسكنة تعادل ثلث فعالية نظيرتها الانحلالية.
- التسكين:
- الأطفال: يعطى فموي أو حقن عضلي تحت الجلد بجرعة 0.5-1 ملغ/كغ كل 4-6 ساعات حسب الحاجة، الجرعة القصوى 60ملغ كل 4-6 ساعات.
- البالغين: يعطى فموي أو حقن عضي تحت الجلد بجرعة 30ملغ (15-60 ملغ) كل 4-6 ساعات حسب الحاجة، الجرعة القصوى 360ملغ/24 ساعة.
- تثبيط السعال: فموي لتثبيط السعال غير المنتج للقشع
- الأطفال بجرعة 1 -1.5 ملغ/كغ/يوم تقسم 4-6 دفعات حسب الحاجة.
- البالغين: 10-20 ملغ كل 4-6 ساعات حسب الحاجة، الجرعة القصوى 120ملغ/24 ساعة.
تعدل الجرعة عند مريض القصور الكلوي (قد يعدل ذلك عند شدة المرض):
- تصفية الكرياتينين 10-50 مل/د: 75% من الجرعة المعتادة.
- تصفية الكرياتينين أقل من 10 مل: 50% من الجرعة المعتادة.
المراقبة
يراقب مدى زوال الألم، والحالة التنفسية والعقلية، والعلامات الحيوية.
ملاحظات
- يجب تجنب تناول مثبطات الجملة العصبية/الكحول خلال فترة الاستخدام بسبب تعاضد التأثير المثبط (تهدئة مفرطة)
- يراقب سكر الدم لأنه يسبب ارتفاع التركيز المصلي للسكر عند تناول الأطعمة الحاوية عليه
- قد يسبب النعاس وقد يلحق الخلل بإنجاز الأعمال التي تحتاج لتركيز ومحاكمة منطقية
- قد يسبب استعماله المديد اعتماد فيزيائي ونفسي ملحوظ
التداخلات المخبرية
يسبب تناوله ارتفاع التراكيز المصلية من SGOT وSGPT
الأشكال الصيدلانية
- محلول معد للحقن: 30ملغ (1مل، 2مل) – 60ملغ (1مل، 2مل)
- محلول معد للتناول عبر الفم: 15ملغ/5ملغ
- أقراص عادية: 15ملغ، 30ملغ، 60ملغ
- أقراص ذوابة: 15ملغ، 30ملغ، 60ملغ
مصادر
كتاب الشامل في الأدوية السريرية، د.محمد عبد الرحمن العينية - د.محمود موسى طلوزي، منشورات دار القدس للعلوم